There’s a common misconception that any medications we can get from a grocery store aisle are harmless. Sure there are some warning labels on the back, but that’s just the fine print — something we skim over to find the dosage. But did you know that you could be putting yourself at serious risk by mixing certain prescription medications, supplements, and substances with over-the-counter medications?
If you didn’t, that’s okay! Most people don’t know that there are any risks associated with over-the-counter medications. But we’re here to help. In this blog, we’re going to cover some common over-the-counter medications and the substances or medications you shouldn’t mix them with. Keep reading to find out more.
Pain Relievers
There are many different types of pain relievers available to purchase at a pharmacy, but most of these belong to the same category of drugs known as NSAIDs. NSAID stands for non-steroidal anti-inflammatory drugs, and includes Ibuprofen (Advil/Motrin), Naproxen (Aleve), and high-dose Aspirin (low-dose Aspirin is generally not considered an NSAID).

Common drug interactions with NSAIDs include alcohol, blood thinners, and select antidepressants, including selective serotonin reuptake inhibitors (SSRIs) and lithium. Mixing more than one type of NSAID at a time can also cause interactions; you should only combine NSAIDs if advised by a medical professional.
An NSAID can stay in the body for up to 10 hours after being taken and alcohol can stay in the body for up to 24 hours after being consumed. If you’re over 21 and are planning on taking an NSAID while or after drinking, check the packaging on your specific medication for advice on minimizing the adverse effects of mixing the two.
Tylenol
You might be surprised to learn that Tylenol (acetaminophen) is another pain reliever that’s unsafe to mix with alcohol. Combining the two is very dangerous and can lead to liver damage.
Some other drug interactions with Tylenol include blood thinners (like warfarin), some seizure medications (like phenytoin and carbamazepine), and some antibiotics (like isoniazid and rifampin).
If you’re over 21, you might be wondering what you can take for a hangover. The best cure is to hydrate, hydrate, hydrate. Drink lots of water or try something like Hydralyte or Liquid IV to speed up the hydration process and boost your body with electrolytes.
Cold Medicines
Dextromethorphan is a decongestant found in many common cold medications such as DayQuil, Mucinex DM, or Robitussin. Dextromethorphan is very dangerous to mix with many antidepressants, including:
- Selective serotonin reuptake inhibitors (SSRIs) like Lexapro or Zoloft
- Serotonin-norepinephrine reuptake inhibitors (SNRIs) like Cymbalta and Effexor
- Monoamine oxidase inhibitors (MAOIs) like Nardil or Parnate
- Tricyclic antidepressants like Elavil and Anafrani
- Serotonin modulators like Desyrel
- Norepinephrine reuptake inhibitors like Wellbutrin
- St. John’s Wort — an herbal supplement that can act as an antidepressant
Dextromethorphan and antidepressants both interact with the neurotransmitters in your brain. If the two are combined, they can cause a potentially life-threatening condition called serotonin syndrome — a surplus of serotonin in your brain. If you are on antidepressants, make sure not to take any cold medications containing dextromethorphan.
Additionally, combining dextromethorphan with ketamine can cause dizziness, drowsiness, confusion, difficulty concentrating, excessive sedation, and respiratory depression (difficulty breathing).
Allergy Medications
Antihistamines are a class of drug that includes most of your common allergy medications (like Benadryl, Claritin, and Zyrtec). Common interactions for antihistamines include alcohol and cold/flu medications.

Alcohol is particularly dangerous when taking an antihistamine that can cause drowsiness. Combining this type of antihistamine with alcohol increases drowsiness and can lead to impaired motor functioning and reaction times, making it risky to drive a car. As a general rule of thumb, don’t plan on driving when taking an antihistamine that causes drowsiness, but if you’re over 21, it is especially important not to drive if you’ve been drinking as well.
Similarly, combining an antihistamine that causes drowsiness with ketamine can cause dizziness, drowsiness, confusion, difficulty concentrating, excessive sedation, and respiratory depression (difficulty breathing).
Combining antihistamines with cold and flu medications can be dangerous since both may contain the same ingredients, or similar ingredients that have the same effect on your body. Consuming too much of an ingredient can cause adverse reactions. Make sure to check the active ingredient list or any potential interactions between medications before combining antihistamines with cold and flu medications.
Ways to Stay Safe
With so many drugs out there, it can be easy to accidentally combine two, or to combine with other substances, without realizing the dangers. The safest thing you can do is always check the interactions between two medications before combining them, and, if you’re over 21, check to make sure it’s safe to drink alcohol with any medications you are taking. Here are some best practices for staying safe when mixing medications and combining them with substances.
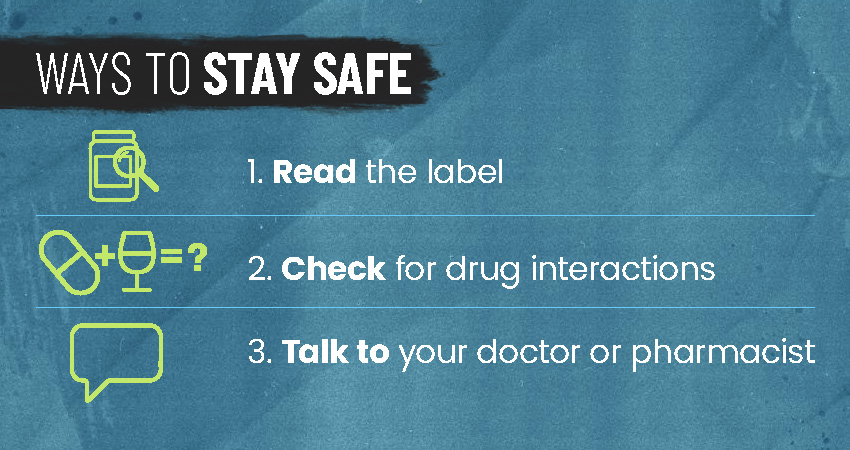
- Read the label. Read the full ingredient list on any medication you are taking as well as the dosage instructions and warning label. Be sure to carefully follow the instructions on the medication to keep yourself safe.
- Check for drug interactions. If you are taking more than one medication, or combining a medication with substances, check for interactions between what you are consuming. One great resource is Drugs.com — here, you can check interactions between almost all drugs, substances, and alcohol. If you are engaging in recreational drug use, be sure to check for interactions as well.
- Talk to your doctor or pharmacist. If your doctor is prescribing you a new medication, be sure to ask what some common drug interactions are. You can also talk to your pharmacist about drug interactions when picking up a prescription. If you are unsure about mixing two over-the-counter medications after checking the interactions online, your doctor or pharmacist is also a great resource to ask.
Resources
- Drugs.com Drug Interaction Checker: A great resource to check interactions between drugs and other substances, food, and alcohol.
- Mixing Recreational Drugs and Alcohol: Details the impacts that combining alcohol has with different recreational drugs.
- The Truth About Mixing Alcohol and Cannabis
- If you or someone you know needs help with substance use, you can call SAMHSA’s national helpline at 1-800-622-HELP (4357).
- The helpline is free, private, and available 24 hours a day/7 days a week for individuals and families experiencing mental health or substance use challenges.
- They can provide referrals and information on local resources, facilities, support groups, and community-based organizations.
- You will not be asked or required to give any personal information.
- You can also visit their website at Samhsa.Gov, or send your zip code via text message to 435748 (HELP4U) to find help near you.
- For more information on available resources, check out our Get Help page.
